| FAQ |
1. |
Brain strokePainless Attack..but equally DANGEROUS |
2. |
Uterine Fibroid Embolization : Preserve WomanhoodFibrolds : Non-cancerous Uterine Tumours |
3. |
Fallopian tube recanalisation : Cherish Womanhood
|
4. |
Peripheral Vascular Disease (PVD)Save Your Limbs – Know About PVD |
Brain stroke
Painless Attack..but equally DANGEROUS
What are Stroke symptoms & signs ?
The symptoms of stroke depend on what part of the brain is damaged. In some cases, a person may not even be aware that he or she has had a stroke.
If you see of have one or more of these symptoms, don’t wait, call your doctor……
- Weakness or loss movement (paralysis) of any part of the body (like an arm, leg, or side of the face)
- Numbness, tingling, or decreased sensation
- Changed or diminished vision
- Language difficulties, inducing slurred speech, inability to speak, inability to understand speech, difficulty reading or writingread more
- Swallowing Difficulties or drooling
- Loss of memory
- Vertigo (abnormal sensation of movement)
- Loss of balance or coordination
- Personality changes
- Mood/emotion changes (such as depression apathy)
- Drowsiness, lethargy, or loss of consciousness
- Uncontrollable eye movement or eyelid drooping
If one or more of these symptoms is present for less than 24 hours, it may be a transient Ischemic Attack (TIA). A TIA is a temporary loss of brain function and a warning sign for a possible future stroke.
What is Stroke ?
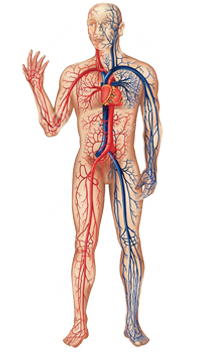
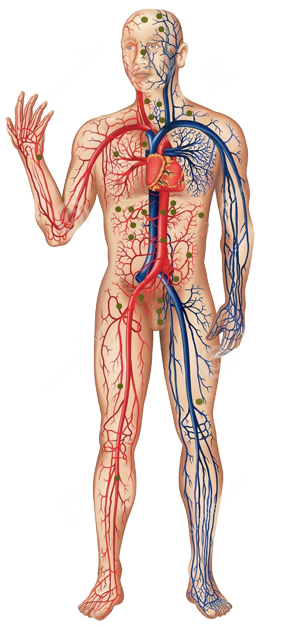
Stroke happens when blockage or breakage of a blood vessel interrupts the blood supply to an area of the brain. Brain cells in the immediate area usually die within a few hours. Strokes can impair speech, vision, movement or memory, depending on where in the brain in happens. Some people recover completely, while others die after very severe strokes. A thrombosis, or blockage in a blood vessel, or an embolism, a fatty deposit or clot which breaks loose and follows the blood stream until it lodges in a smaller vessel, can literally cause the brain to starve to death in a very few minutes by depriving it of blood & thereby oxygen to tissue.
What are Lab Tests and procedures Used for Stroke Diagnosis ?
Here are the tests doctors uses most often in stroke diagnosis.
- CT Scan to know clot or bleeding
- Angiography to view the Blood Vessels that supply the Brain
- Tests that View the Heart or Check its Function
- Routine Screening Tests
- Other Neurologic Tests
What are treatment for Stroke ?
A stroke is a medical emergency. Physicians have begun to call it a “brain attack” to stress that getting treatment immediately can save lives and reduce disability. Treatment varies, depending on the severity and cause of the stroke. For virtually all strokes, hospitalization is required, possibly including intensive care and life support. The goal is to get the person to the emergency room, determine if he or she is having a bleeding stroke or a stroke from a blood clot, and begin appropriate therapy within 3 hours.
Immediate treatment
Thrombolytic medicine, like Urokinase tPA, breaks up blood clots and can restore blood flow to the damaged area. People who receive this medicine are more likely to have less longterm impairment. However, there are strict criteria for who can receive thrombolytics. The most important is that the person be evaluated and treated by a specialized stroke team including neurologist and Intreventional Radiologist. Vascular & Interventional Radiologist is a specially trained physician in vascular diseases, who will perform Cerebral angiography through a small puncture made in artery to locate the blood vessel with tiny micro catheter and release clot bursting thrombolytic agent at the site of clot, thereby preventing systemic side effect of this agent. He would do periodic check angiogram to know the status of clot within 3 to 5 hours of when the symptoms start.
Uterine Fibroid Embolization : Preserve Womanhood
Fibroids : Non-cancerous Uterine Tumours
Do you suffer from the following symptoms ?
- Heavy bleeding
- Perlvic pain
- Anemia
- Frequent urination
- Difficult or painful bowel movements
- Swollen or distended abdomen
- Difficult or painful bowel movements
- Swollen or distended abdomen
- Difficulty getting or staying pregnant
There are chances that you may be suffering from Fibroids.
Uterine fibroids are the most common tumor of the female genital tract. They are not concerous (benigs) growths that develop in the smooth muscle layers within the uterus. 40% of all women over 35 have fibroids.
What are the Causes ?
- The Factors that cause the fibroids to grow in the uterus are not known. They grow under the influence of female hormones.
- All most all fibroids occur in women of reproductive age.
How Fibroids are diagnosed ?
Usually, diagnosis of fibroids occurs during a gynecological examination where the Gynecologist feels the fibroids during a physical exam.
This is often confirmed with ultrasound, or in some cases
Does having uterine fibroids mean that woman would be intertile or unable to have children ?
In some cases, fibroids can prevent a woman from getting pregnant through natural methods.
What are the Treatment Options ?
Usually, medical management is the first therapy for uterine fibroids. Medical therapy includes treatment with non steroidal anti inflammatory agents Birth control pills or progesterone agents may also be utilized.
Another medication that may be used in certain circumstances is Gonadotropin releasing hormone agonistic (GnRH). Commonly, these drugs cause symptoms similar to those in patients experiencing menopause. These include not flashes, as well as mood changes. They can also cause some more serious side effects, such as osteoporosis, or a decrease in a density of the bones. Thus, their use is usually limited to approximately 6 months. Unfortunately, fibroids usually regrow after this period of time.
Surgical Therapy
Myomectomy removes only the fibroids and leaves the healthy areas of the uterus in place. This procedure can preserve a woman’s ability to have children. However in some cases, the gynecologist may not feel that a myomectomy is appropriate due to the possibility that it will cause pelvic scarring.
Unfortunately, approximately 30% of the fibroids do regrow and cause a recurrence. In these case the gynecologist may recommend alternative therapies such as fibroid immobilization.
Hysterectomy is used when a woman’s fibroids are large, or has heavy bleedings, and she is either near or past menopause, or completed her family. In general, recovery time from a hysterectomy is one to two months.
Uterine Artery Embolization
Uterine Artery Embolization is a procedure performed by an Interventional Radiologist. An Interventional Radiologist is a physician who specializes in using imaging guidance to perform minimally invasive procedure to treat different diseases Small puncture made here. Catheter fed into femoral artery. X-ray imaging locates blood vessels. Tiny paarticles are injected. Colour nourishing tumor are blocked fibroid begins to shrink.
Thus, the only thing the patient should feel during the examination is the initial numbing and the remainder of the procedure should be painless. After embolization medications will be required for control of post embolization pain.
What are the Success Rates ?
- 99% of patients experience immediate relief from heavy bleeding
- 94% of patients experienced 50-60% DShrinkage
- 335 of patients who attempted to conceive are successful
- 99% of patients returned to work within less than a week
- The size of the fibroids usually decrease approximately 40-70% in 6 months and greater at a year.
One major advantage of uterine embolization is that it is a global treatment in that it treats every fibroid in the uterus. This procedure also enjoys a very low serious complication rate of less than 1%.
What are benefits of Flbroid Embolization ?
- 94% success rate (per 1000 patients)
- Fibroids which are embolized do not recur
- Short recovery time
- Local anesthesia
- Uterus is not cut open, scarned or removed (versus hysterctomy)
- Fertility & womanhood is maintained
- Immediate reduction of symptoms
- Patients under 40 who wanted to conceive, one third conceived & delivered normally
- Most experienced a normal pregnancy.
Fallopian tube recanalisation : Cherish Womanhood
Fallopian tube recanalisation
You and your partner have been trying to conceive but have been unable to do so. You probably have undergone several tests and examinations for infertility workup and have learned that there is a blockage in one or both of your fallopian tubes. There are chances that your doctor may suggest you to undergo “Fallopian Tube Recanalization”. This is an x-ray procedure in which a special catheter is used to open the fallopian tubes. read more
Why do I need Fallopian tube recanalisation ?
Other tests will have shown that one or both of the tubes leading from your ovaries to the uterus have become blocked. This may well be preventing you from conceiving. It is possible that you may require an operation to try and unblock the tubes, but Fallopian tube recanalisation may be all that is necessary.
Who does follopian tube recanalisation ?
A specially trained doctor called a Interventional radiologist. Interventional radiologists have special expertise in using x-ray equipment, and also in interpreting the images produced. They need to look at these images white carrying out the procedure.
Where will the procedure take place ?
In the Catheterization lalboratory.
Are there any risks or complications ?
Fallopian tube recanalisation is a very safe procedure, but there are some risks ad complications that can arise. Perhaps the biggest problem is that the procedure is unsuccessful, and it does not prove possible to unblock the Fallopian tubes. Very rarely, infection can be introduced into the inside of the pelivs, but this can generally be treated satisfactorily with antibiotics.
When in the menstrual cycle should the Fallopian tube recanalization be performed ?
It should be performed at approximately day six to eleven of the menstrual cycle which is after the cessation of menses and before ovulation.
What are the indications and contraindications to fallopian tube recanalization (aka. Tuboplasty) ?
A proximal fallopian tube occlusion is often due to the accumulation of mucus or debris forming a plug in the proximal portion of the tube. This may happen in both tubes or simply in one of the two fallopian tubes. Patients with a proximal occlusion benefit from the Fallopian tube recanalization procedure.
In fact, the American Society for Reproductive Medicine has recommended that patients who have proximal tubal obstruction undergo this procedure prior to any other more invasive procedures.
The contraindications of the procedure are active uterine bleeding, active pelvic infection, recent surgery and current pregnancy.
How long will it take ?
Every patient’s situation is different, and it is not alwlays easy to predict how complex or how straightforward the procedure will be. It may be over in 20 minutes. As a guide, expect to be in the Cath-Lab for about an hour altogether.
What are the results associated with the fallopian tube recanalization?
If potency can e restored during the procedure which occurs in approximately 65-90 percent of cases reported conception rates in the literature are approximately 33 percent. A small proportion of the patients re occlude their Fallopian . A small proportion of the patients re occlude their Falloplan tubes and require repeat procedure about 8 months to 1 year later.
What are the potential complications of Fallopian tube recanalization?
Serious fallopian tube recanalization complications are extremely rare. Mild bleeding and fallopian tube perforation can occur but are usually without sequel. Infections and contrast reactions can occur as well but again are very rare. Sometimes after fallopian recanalization there is slight increased risk of an ectopic pregnancy (Tube Pregnancy).
What are the results of Fallopian Tube Recanalisation ?
The results of this new procedure are encouraging; fallopain tube recanalisation has been successful in a large percentage of patients undergoing the exam.
To date, no serious complications have resulted from this procedure. The procedure generally takes less than one hour and often is completed in less than 20 minutes.
The radiation dose to the overies is kept to a minimum and during this phase of the menstrual cycle, it does not pose a risk of fetal information.
Finally …
Some of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion about your treatment with the doctors looking after you.
Fallopian tube recanalisation is considered a very safe procedure, designed to save you having a larger operation. There are some slight risks and possible complications involved, and although it is difficult to say exactly how often these occur, they are generally minor and do not happen very often.
Peripheral Vascular Disease (PVD)
Save Your Limbs – Know About PVD
If you have the following/ then you must read about PVD and save your limbs.
- (A) Diabetes
- (B) Hypertension
- (C) Over weight
- (D) High cholesterol
- (E) Smoking/tobacco chewing
- (F) Previous or family history of Heart or Vascular disease
- (G) Age over 40
(A) What is peripheral vascular disease?
PVD is a condition in which the arteries that carry pure oxygenated blood to the arms or legs becomes narrowed or blocked interfering with normal flow of blood to the muscle of limbs.
The most common cause of PVD is atherosclerosis (often called hardening of arteries) Atherosclerosis is the gradual process in which cholesterol and scar tissue build up forming a substance called “plaque” that blocks blood vessels. PVD may also be caused by blood clot.
B) What are the symptoms of PVD?
- Leg or hip pain on walking
- Pain stops on resting
- Numbness/Tingling
- Weakness in leg
- Burning or aching pain in feet or toes when resting
- Sore or ulcer on leg or foot that won’t heal
- cold legs or feet
- Color changes in skin of legs or feet
- loss of hair on legs
(C) How PVD is diagnosed?
The most common is clinical Examination by Physician, Peripheral pulse at ankle, foot, and knees or at groin is absent or weak. Next is ankle-brachial index of blood pressure i.e. the pressure in your foot is compared to the pressure in your arm to determine how well your blood is flowing in your foot and what further tests are needed.
(D) How is PVD being treated?
The best treatment depends on the number of factors including your overall heath and severity of disease. In some cases life style changes are enough to half the progress of PVD and manage the disease. your physician or Interventional Radiologist may prescribe drugs when life style changes are not enough. Procedures that open blocked blood vessels also are used to treat PVD.
Life style changes:
Most important plan will include plan will include a low fat diet and a program of regular exercise. If you are a smoker it is absolute essential that you stop all types tobacco. If decreased blood flow to the legs is carrying numbness and tingling then injury to feet and toes needs to be avoided. Injury to feet and toes occur then a foot care programme to prevent sores infection may be prescribed. This may include referral to a podiatrist.
Medication:
Medication that lowers cholesterol or control high blood pressure may be prescribed. Medication also is available that has been shown to significantly increase pain-free walking distance and total walking distance in people with intermitted claudicating. Other medication that help prevent blood clots or build up of plaque in the arteries are available, as well.
E) what can be done to treat PVD? when life style changes and medications are not enough?
There are a number of ways that Interventional Radiologist can open the blocked or narrowed blood vessels to restore normal blood flow. There procedures are done without surgery using modern interventional techniques.
Interventional Radiologist are Specially trained physician who use tiny tubes called catheters, other miniaturized tools like guide wire, balloons, stents, aspiration devices under x-ray control to perform these sophisticated procedure
Procedures performed by Interventional Radiologist include :
- Angioplasty : a balloon is inflated to open a narrow blood vessel.
- Thromobolytic Therapy ( at local site of thrombus or clot) : Clot bursting or did dissolving drugs is delivered to the site of blockages caused by blood clots with a specialized pulse spray catheter.
- Stents ; a tiny kink resistant metallic cylinder of steel or Nitinol alloy is inserted in the blocked blood vessel to act like scaffolding and hold it open.
- Stent Graft ; a stent covered with symthetic fabric is inserted into the blood vessels to bypass diseased arteries. Some times open surgery is required to remove blockages from arteries or to bypass the blocked area. Vascular surgeons perform these procedures.
(F) How can I find out, if I have PvD ?
If you suspect that you may have Pvd it is important that you see your personal physician/Interventional radiologist for an evaluation at the earliest, so that further complications like rest pain, non healing ulcer, gangrene can be prevented and limbs can be saved.
(G) Who is an Interventional radiologist ?
Interventional radiologists are physicians who have special training to diagnose and treat conditions using tiny miniature tools while watching their progress on X-ray /cath. lab equipment. Typically Interventional Radiologist performs procedures through a very small nick in the skin about the size of a pencil tip. Interventional radiology treatments are generally easier for patients that surgery because they involve no surgical incisions, less pain and shorter hospital stay, Your interventional radiologist will work closely with you physician to assure that you receive the best possible care.